
Imagine a nurse on a quiet night shift who suddenly senses that something isn’t right—an almost imperceptible change in a patient’s condition that signals an urgent need for attention.
This is patient acuity in action. In today’s fast-paced healthcare environment, understanding the severity of a patient’s illness or medical condition isn’t mere theory—it’s the difference between a well-timed intervention and a crisis.
Let’s explore how patient acuity transforms patient care and how immersive clinical simulation in nursing sharpens nurses’ instincts for those split-second decisions.
Understanding Patient Acuity
Patient acuity quantifies the intensity of care a patient requires. It is a concrete, actionable measure that helps a nurse decode the urgency hidden within every patient’s presentation.
Measurable Impacts of Patient Acuity
Patient acuity tells you precisely how much care is needed. A low acuity case might require vigilant monitoring, while a high acuity scenario demands immediate intervention. Sage Journals reveal that higher patient acuity significantly increases the likelihood of missed nursing care, which can lead to delays in treatments, prolonged hospital stays, and complications (Lake et al., 2018). Properly adjusting staffing to account for acuity not only reduces the odds of missed care but also improves patient outcomes and mitigates nurse burnout.
- Acuity-Adjusted Workload: A 1 standard deviation increase in acuity-adjusted workload doubles the odds of missing care and adds 0.6 more missed activities on average.
- Impact on Hospital Stays and Complications: Missed care, such as delayed feedings, leads to longer hospital stays and complications like necrotizing enterocolitis.
- Missed Care and Patient Acuity: A 1 standard deviation (SD) increase in patient load resulted in a 75% increase in the odds of missed care. A 1 SD increase in patient acuity increased the odds of missed care by 47%.
- Work Environment Improvements: Enhancing the work environment by 1 standard deviation reduces the odds of missed care by 34%.
- Missed Activities Prevalence: Common missed activities include patient comfort (12.5%), breastfeeding support (10.6%), and timely discharge preparation (9.9%).

Unexpected Turns
Even patients initially classified as low acuity can suddenly deteriorate. Recognizing early warning signs transforms uncertainty into calm, decisive action. This is where building confidence in nursing through precise training makes all the difference.
Low Acuity vs. High Acuity: Real-World Scenarios
Let’s break down these scenarios with clear, relatable examples:
Low Acuity Patients
Low acuity patients are those whose conditions require minimal immediate intervention but still demand careful monitoring to prevent escalation.
These cases often include mild symptoms like a common cold, minor injuries, or early-stage infections. However, even routine conditions can escalate.
For example, an untreated urinary tract infection (UTI) in an elderly patient can lead to urosepsis, a life-threatening condition. Similarly, what seems like a simple cold in a child could develop into respiratory syncytial virus (RSV) during peak seasons. The CDC’s Antibiotic Stewardship guidelines emphasize early diagnosis and treatment to prevent mild infections, such as community-acquired pneumonia, from worsening (Centers for Disease Control and Prevention, 2024).
Thus, with low acuity cases, early detection and proactive management are your most powerful tools.
High Acuity Patients
High acuity patients, on the other hand, are those whose conditions demand immediate, intense medical intervention due to the severity of their illness or injury. A myocardial infarction (MI) or acute respiratory failure can escalate within minutes, making rapid, instinctive responses critical.
For instance, irreversible heart damage begins within 20–40 minutes of an MI if blood flow isn’t restored, emphasizing the urgency of door-to-balloon time in cardiac emergencies (Thygesen et al., 2018). Similarly, in acute respiratory distress, delayed oxygen therapy or intubation can lead to multi-organ failure.
Training is key. Realistic simulations build muscle memory, ensuring rapid, life-saving decisions in high-stakes situations.
For more detailed strategies on handling high-acuity scenarios, check out our related post on how nurses can train for high-acuity scenarios.
Challenges in Managing Patient Acuity
Navigating the healthcare environment means dealing with several challenges that test your skills daily:
- Understaffing and Pressure: When nurse-to-patient ratios are off, even minor oversights can quickly escalate. The precise evaluation of patient acuity is essential to safely distribute your attention where it’s needed most.
- Rapid Decision-Making: High acuity scenarios force you to make critical decisions in seconds, not hours. The ability to translate training into confident, immediate responses is vital.
- Building Confidence in Nursing: Every challenging case is a lesson in resilience. With practical, hands-on training, particularly through immersive clinical simulation in nursing, you develop the muscle memory necessary to transform uncertainty into assured action.
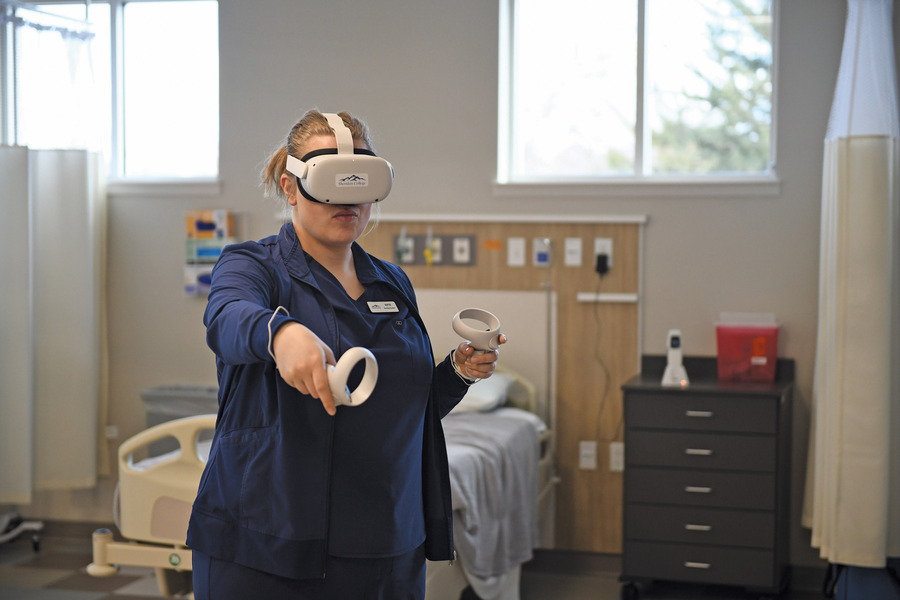
Transforming Training with Immersive VR Simulation
Just like a pilot drilled for High Acuity, Low Occurrence (HALO) events, nurses can now harness immersive virtual reality (VR) training to prepare for the unexpected. Platforms like UbiSim offer targeted simulations that equip you with the skills to manage cases ranging from low to high acuity.
Benefits of Immersive VR Training
- Specific, Real-World Scenarios: VR simulation replicates a broad array of patient acuity cases. For instance, you can practice managing a diabetic ketoacidosis (DKA) case or responding to a myocardial infarction scenario—all within a controlled environment.
- A Risk-Free Space for Mastery: In VR, mistakes become valuable lessons without real-world consequences. This safe space allows you to repeat complex scenarios until your responses are polished and instinctive.
- Unmistakable Realism: Cutting-edge VR technology creates immersive experiences that mirror the realistic sounds, visuals, and pressures of an actual clinical scenario—from the beeping of monitors to the palpable urgency in high-pressure moments.
- Consistency and Repetition: With VR, you can continuously practice the same scenario until you achieve mastery. Repetition is key to embedding the knowledge and skills required to effectively manage patient acuity in any situation.
- Cost-Effectiveness and Scalability: Beyond the immediate training benefits, VR offers a scalable solution that institutions can customize to their needs. This method not only streamlines training costs but also ensures a consistent standard of care across your team.
Final Thoughts
Patient acuity is the silent heartbeat of quality nursing care. It guides every decision—from low acuity alerts that require careful monitoring to high acuity emergencies demanding immediate, decisive action. By mastering this essential concept and embracing innovative tools like immersive VR training, you empower yourself to transform ordinary shifts into moments of extraordinary patient care excellence.
Clear, concrete scenarios coupled with practical, repeated training ensure that when the unexpected unfolds, you’re not just prepared—you’re confident in your ability to act decisively. In a field where every second counts, how are you honing your skills to make that critical difference?
References
Centers for Disease Control and Prevention (CDC). (2024, April 12). Core Elements of Antibiotic Stewardship. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/antibiotic-use/hcp/core-elements/index.html
Lake, E. T., Staiger, D. O., Cramer, E., Hatfield, L. A., Smith, J. G., Kalisch, B. J., & Rogowski, J. A. (2018). Association of Patient Acuity and missed nursing care in U.S. neonatal intensive care units. Medical Care Research and Review, 77(5), 451–460. https://doi.org/10.1177/1077558718806743
Thygesen, K., Alpert, J. S., Jaffe, A. S., Chaitman, B. R., Bax, J. J., Morrow, D. A., & White, H. D. (2018, October). Fourth Universal Definition of Myocardial Infarction. JACC Journals. https://www.jacc.org/doi/10.1016/j.jacc.2018.08.2140


John pens stories on the rapidly changing landscape of VR in nursing simulation. John is committed to elevating the voices of practicing nurses, nurse educators, and program leaders who are making a difference.
Explore more

Top 5 Signs Your Nursing VR Sims Aren't Immersive
If learners are clicking menus instead of making decisions, your VR nursing sims may lack immersion. Here are 5 red flags—and what to look for instead.
Is Your Nursing VR Experience Hitting the Mark? Here’s How to Tell
Is your nursing VR truly immersive? Discover how to tell if your simulation empowers learners to think, act, and feel like real nurses every step of the way.

Nursing Simulation Decisions: Manikin Programming vs. VR Custom Scenarios
Compare manikin-based vs. VR nursing simulations. Discover how UbiSim empowers educators to create immersive, customizable, real-world scenarios.