
Maybe it’s the floating menus. Or the click-heavy interface. Or that nagging feeling that your students are going through the motions rather than truly stepping into the role of the nurse.
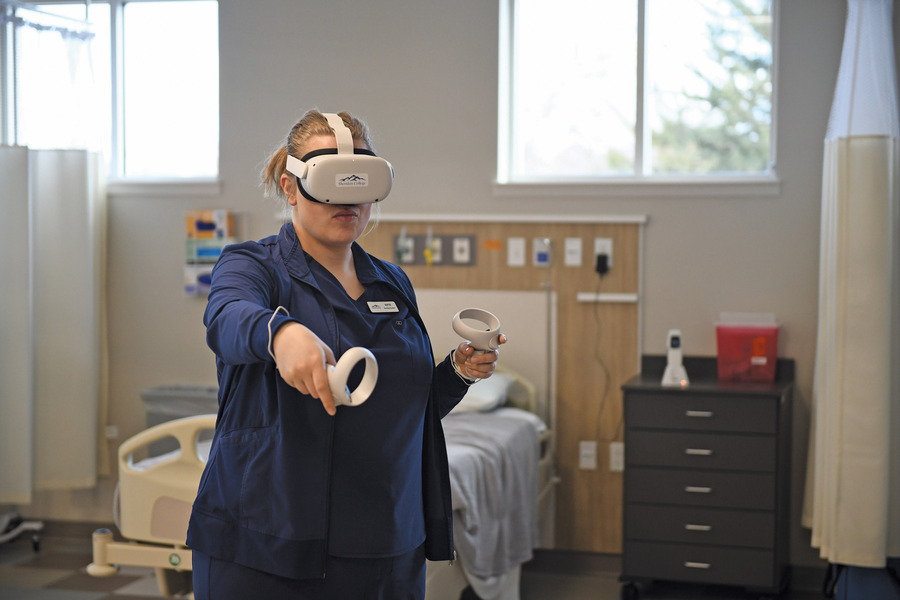
In nursing simulation, immersion refers to the degree to which a learner feels fully engaged and present in a simulated clinical environment, suspending disbelief and acting as if the simulation is real. It’s what turns a headset into a hospital room, a virtual patient into someone who needs their care, and a learner into a confident, decision-making nurse.
Immersion isn’t just a nice-to-have—it’s a predictor of student performance. Research shows that immersion, defined as strong student engagement and a feeling of joy, is a critical factor in successful learning and has been found to directly correlate with academic achievement in immersive simulation environments (Thapa et al., 2024).
But not all VR experiences are created equal. Not all are immersive.
When done right, immersive VR enhances clinical judgment, fosters psychological safety, and makes learning stick. When done poorly, it creates confusion, anxiety, and detachment—ultimately undermining the very outcomes it’s supposed to support.
So, how can you tell if your VR simulations are truly hitting the mark?
Here are the top five red flags that your VR platform might be failing, and what to look for in platforms like UbiSim to ensure your learners are thinking and acting like nurses.
1. Learners Are Navigating Menus, Not Caring for Patients
If your students are spending more time clicking through menus than engaging in patient care, something’s off. When a learner has to scroll through a pop-up menu to “select” a blood pressure cuff instead of physically picking it up, the moment loses its realism. Instead of thinking about the patient’s vitals, they’re thinking about the interface.
What to look for instead: A simulation platform that feels natural and mirrors real clinical practice. In UbiSim, the learner physically reaches for the blood pressure cuff, wraps it around the patient’s arm, and hears the reading through the stethoscope. Your learners should be thinking like nurses—interacting with the patient and environment the way they would in real life.
2. Learners Are Afraid to Make Mistakes
Immersion isn’t just about realism. It’s also about psychological safety. If your students feel anxious about messing up in front of their peers because they’re struggling with the tech, they’re less likely to take risks, ask questions, or engage fully. In some platforms, if a learner makes an incorrect choice (choosing the wrong medication), they end the simulation immediately or mark it as a failure on the spot without giving the learner a chance to recover or reflect within the scenario.
What to look for instead: A simulation experience that promotes psychological safety by allowing learners to make mistakes. UbiSim offers natural, real-time feedback through evolving patient cues, like changing vital signs, lab results, or provider calls, just as they happen in real clinical settings. This in-scenario feedback nudges learners to reassess and adapt, rather than interrupting the flow. After the scenario ends, structured evaluative feedback—like a performance report—helps reinforce learning by highlighting missed steps and encouraging reflection. This combination of in-the-moment clinical cues and post-sim analysis supports deeper understanding while preserving the learner’s confidence and autonomy.
Dean Dr. Erin-Joy Bjorge at the Buntain School of Nursing at Northwest University said about her students,
“With VR, those barriers go away in the sense that students lose the embarrassment, even if they make a mistake. As a result, they felt more prepared as they walked into the high-fidelity sims. Of course, it was the same scenario, but they felt more prepared because they’d been able to practice without fear of making a mistake or being embarrassed in front of their peers.”
3. Learners Are Talking About the Platform, Not the Patient
One of the clearest red flags is when learners ask, “How was I supposed to open the cart again?” If the post-sim discussion is dominated by technical confusion rather than clinical reflection, your VR platform is getting in the way.
What to look for instead: Learners who come out of a simulation immersed in the patient’s story, eager to unpack their decisions and discuss what they might do differently next time. They should be asking questions like, “Did I miss a critical change in vitals?” or “Was that the right intervention for early signs of sepsis?” because the technology faded into the background and let the clinical learning take center stage.
4. Learners Feel the Scenario is Scripted, Not Real
In low-immersion VR, it can feel like learners are just following a checklist. For example, a learner might be prompted to “click to administer medication” after a vitals alert, with no opportunity to assess the patient, consider alternate interventions, or escalate care. There’s little room for clinical judgment, critical thinking, or adapting to a changing situation, because the experience is built around fixed responses and pre-programmed outcomes.
What to look for instead: A platform that fosters clinical judgment, flexibility, and realism. In UbiSim, the scenario doesn’t wait for a checklist to be completed. It evolves in real time based on the learner’s actions. For example, if a learner is caring for a pediatric patient showing subtle signs of sepsis, like an increased heart rate, delayed capillary refill, or changes in skin tone, they must actively interpret these cues, reassess the situation, and decide whether to escalate care or administer fluids. There are no pop-up prompts or scripted next steps; the simulation puts the learner in charge, just like in real clinical practice.
Nursing student Euphema Ishola from Bow Valley College shared her experience of UbiSim:
“At the end of the day, I felt like a real nurse.”
5. Learners Aren’t Retaining or Applying What They Practice
When the VR experience is too passive, overly guided, or doesn’t encourage active decision-making, learners may go through the motions without truly internalizing the “why” behind their actions. That’s when you start seeing knowledge gaps resurface during in-person assessments or patient care.
What to look for instead: A good VR system prepares learners well for other high-fidelity sims and clinical practice. The goal isn’t just to complete a scenario—it’s to truly understand the “why” behind each action. Why does a patient need insulin? What cues led to that? What other interventions might have been appropriate? An immersive simulation presents a dynamic situation that requires them to pause, assess, and think like a nurse.
Nicole Manley, MSN, RN, CHSE, CA-SANE, Interim Director, Learning Enhancement & Academic Progress (LEAP) at the University of Texas at Austin, shared:
“VR helps learners prepare and feel more confident going into clinicals—it’s a supplement, not a substitute.”
The best VR platforms reinforce foundational knowledge while developing clinical judgment, so learners walk into the sim lab and the hospital with the tools they need to succeed.
Final Thoughts
At the end of the day, if your learners aren’t thinking like nurses, what is the point? Thinking like a nurse starts with feeling like a nurse in an immersive experience that enables learners to suspend disbelief and engage with the scenario. True immersion is when learning sticks and future nurses thrive.
References
Thapa, S. B., Ramsingh, T. T., Yoo, M. S., & Kim, J. H. (2024). Development and evaluation of an immersive virtual reality simulation to enhance the safety competency of nursing students in medication administration. Nurse Education Today, 129, 105974. https://doi.org/10.1016/j.nedt.2024.105974


As an integral center of UbiSim's content team, Ginelle pens stories on the rapidly changing landscape of VR in nursing simulation. Ginelle is committed to elevating the voices of practicing nurses, nurse educators, and program leaders who are making a difference.
Explore more
Is Your Nursing VR Experience Hitting the Mark? Here’s How to Tell
Is your nursing VR truly immersive? Discover how to tell if your simulation empowers learners to think, act, and feel like real nurses every step of the way.

Nursing Simulation Decisions: Manikin Programming vs. VR Custom Scenarios
Compare manikin-based vs. VR nursing simulations. Discover how UbiSim empowers educators to create immersive, customizable, real-world scenarios.

Key Trends in Nursing Education in 2025
Discover the top 10 trends transforming nursing education in 2025 from VR and AI to telehealth, CBE, and the urgent focus on real-world nurse readiness.