Collaborative Teaching Strategies in Nursing Education: A Modern Approach to Training Nurses
.jpeg)
Table of Contents
Name of the heading
1- Start your table with the syntax {start-table}
2 - Add an H3 Heading to create a new column (this will be the column title)
3 - List cells as bullet points in a List element
4 - End your table with the syntax {end-table}
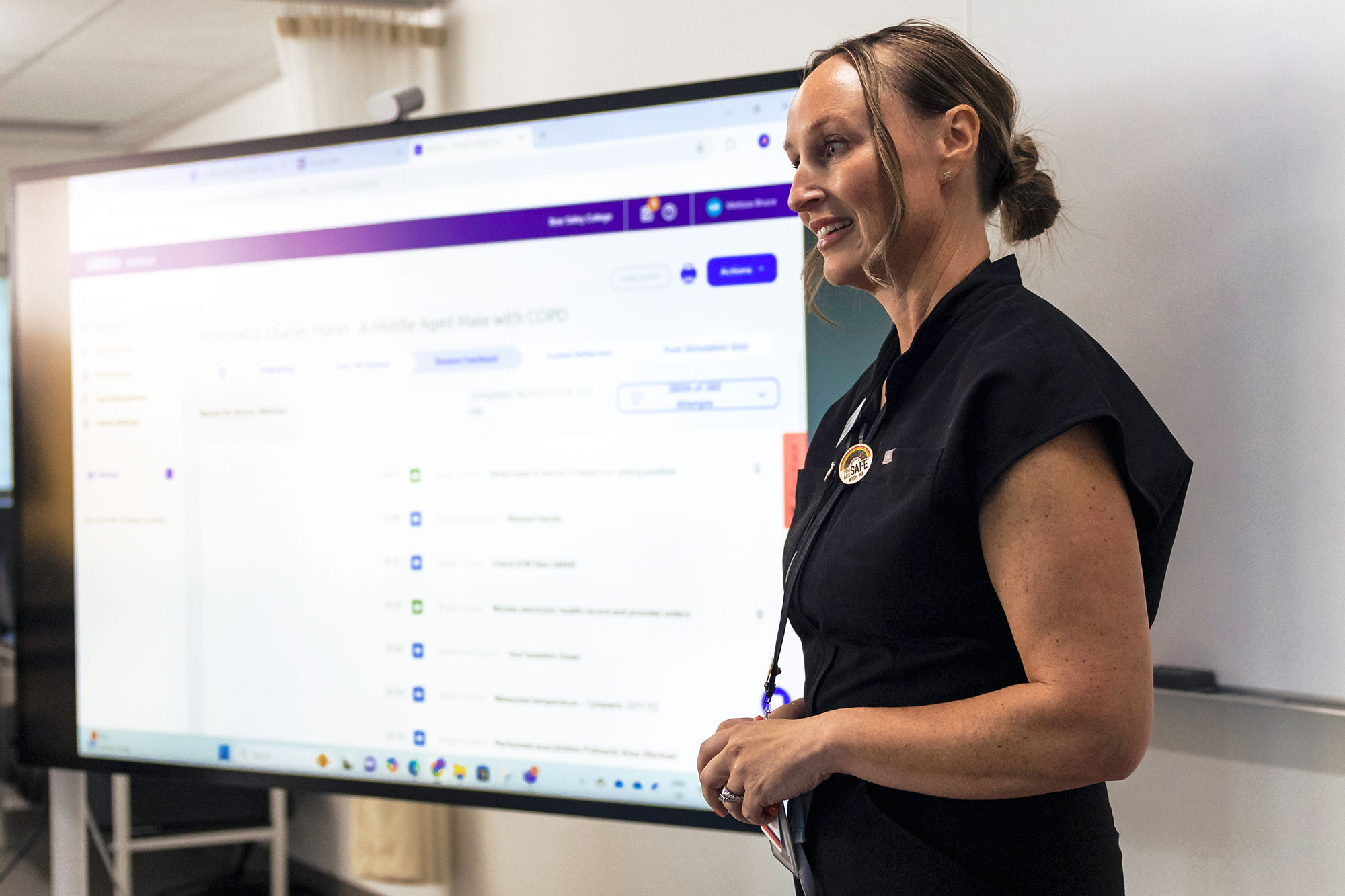
What unites virtual reality, problem-based learning, and role-playing in the nursing education landscape? It's their game-changing potential to transform how nursing students collaborate and learn. As educators in the nursing field, incorporating these collaborative approaches can not only make learning more interactive but can also enhance the quality of education, preparing students for the complexities of healthcare practice.
Simulation Labs: More Than Just Manikins
Simulation labs serve as specialized training grounds where students can hone their clinical skills in a controlled, safe environment. These labs often come equipped with medical mannequins and state-of-the-art software to mimic real-world healthcare situations. Students can role-play as nurses, patients, or family members, practicing essential tasks such as administering medication, performing CPR, or conducting patient assessments.
A recent study corroborates the effectiveness of this approach, suggesting that technology and simulation-based strategies boost student engagement and contribute to a more active learning environment.
UbiSim: Virtual Reality Meets Nursing Education
Within the sphere of simulation labs, UbiSim offers a uniquely immersive experience. This virtual reality platform, designed specifically for nursing education, allows for peer-facilitated learning. One student provides cues from a virtual patient or their family member, while another wearing the VR headset must respond to these prompts. This interactive setup enhances clinical judgment skills, prepares students for the Next Gen NCLEX, and simulates real-world clinical practice.
Peer Teaching: A Two-Way Learning Street
Students are paired together or placed in small groups, taking turns to act as both the teacher and the learner. This facilitates a mutual learning experience, allowing students to learn from each other’s strengths and weaknesses. By teaching a subject, the 'peer teacher' reinforces their own knowledge and gains valuable experience in explaining complex topics. Meanwhile, the 'peer student' benefits from a different perspective and perhaps a simpler or more relatable explanation than what an instructor might provide.
Case Studies: Tackling Real-World Scenarios Together
Incorporating case studies into the nursing curriculum empowers students to collaborate on solving real-life healthcare challenges. They apply theoretical knowledge to clinical contexts, practice decision-making, and engage in analytical discussions. Case studies stimulate critical thinking and collaborative problem-solving, making them an essential asset in nursing education.
Problem-Based Learning (PBL): Empowering Proactive Learning
In a PBL setting, students are given complex health problems to solve collaboratively. Rather than being a lecture-based approach, this strategy encourages students to seek out information and solutions actively. They must employ critical thinking, research skills, and collective brainstorming to address these issues effectively. A study found that “PBL appears to improve nursing students' critical thinking skills, especially their ability to analyze and evaluate.”
Role-Playing: Stepping into Others' Shoes
Role-playing exercises immerse students in simulated healthcare scenarios where they take on the roles of various stakeholders—be it nurse, patient, or family member. These exercises offer a window into the multifaceted responsibilities and challenges inherent to each role. Consequently, role-playing not only cultivates empathy but also equips students with the multi-disciplinary teamwork skills vital to real-world healthcare settings.
One study specifically highlighted that role-playing was effective in improving the empathy scores of operating room nursing students. Empathy isn't just an innate trait but can be cultivated through targeted education.
Conclusion
By melding traditional teaching methods with innovative strategies such as UbiSim, educators can offer a more dynamic, hands-on, and collaborative learning environment, thereby shaping competent and empathetic nursing professionals for the future.
FAQs
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
Explore more

Why Q1 Decisions Determine Your Nursing Workforce Pipeline
Why January–March decisions shape nursing workforce capacity, readiness, and retention, and how early action strengthens the pipeline.

From 30 Minutes to 3: How AI Enhanced Analytics Transforms Debriefing Preparation
AI Enhanced Analytics: Scenario Performance Data now available in UbiSim's Version 1.19
.jpg)
Behind the Scenes: How We Brought Incisions & Dressings to Life in VR
How the UbiSim team built a VR system displaying 300+ distinct incision states—balancing clinical accuracy, technical constraints, and nursing education needs.